Help Seeking
Here are people you can call
Although many men do seek help the most common finding in the help seeking literature is that they seek help less often and at a later stage.
The first place people look to for help is from their friends, families, colleagues or wider communities. Often this can be enough to resolves difficulties as and when they arise. Unfortunately, men have fewer supportive relationships and the quality of help from these relationships may not be as good as it could be.
The last place people turn to for help is from professionals but many people with psychological problems report never having used professional mental health and well-being services. Psychological services need to be more accessible and more needs to be done to develop services that men would like to receive support from.
Technical Stuff
One of the most common findings in the help seeking literature shows that females are more likely to seek help for mental and physical health problems than males (Addis & Mahalik, 2003; Blazina & Watkins, 1996; Good, Dell & Mintz, 1989; McKay, Rutherford, Cacciola & Kabasakalian-McKay, 1996; Mahalik, Good & Englar-Carlson, 2003; Padesky & Hammen, 1981; Thom, 1986; Willis, Fabian & Hendershot, 2005).
Men of different ages, nationalities, and ethnic backgrounds seek help from mental health services less frequently than women from comparative groups (Addis & Mahalik, 2003; Gove, 1984; Gove & Tudor, 1973; Greenley & Mechanic, 1976; Howard & Orlinsky, 1972; Vessey and Howard, 1993). W
hilst sex differences are helpful in highlighting men‟s underutilisation of services they tell us very little about within group differences or the underlying biological, psychological, or cultural processes (Addis & Mahalik, 2003; Mechanic, 1978). Moreover, male versus female comparisons run the risk of supporting essentialist interpretations of gender (Addis & Mahalik, 2003).
One of the most common reasons for not seeking help for psychological difficulties is related to stigma attached to mental illness (Vogel & Wade, 2009).
The threat to an individual‟s self worth and how the person perceives the act of seeking help is also of importance (Vogel, Wade & Haake, 2006).
People from different ethnic groups show different help seeking attitudes (Abramowitz & Murray, 1983; Gonzalez, Alegria & Prihoda, 2005) and across ages help seeking varies (Gonzalez et al., 2005).
Illness perceptions impact on help seeking behaviour (Leong & Zachar, 1999) as does a person‟s locus of control (Fischer, 1970).
Education has been associated with help seeking (Tijhuis, Peters & Foets, 1990) as have individual coping styles (Skeate, Jackson, & Jones, 2002) and selfconcealment (Cepeda-Benito & Short, 1998).
Psychological and social factors appear to have the greatest impact on men‟s help seeking behaviour (Doyal, Payne & Cameron 2003; Courtenay, 2003, 2009; MHF, 2010) with many authors claiming that men‟s help seeking behaviour can be directly related to the social construction and cultural representations of masculinities (Addis & Mahalik, 2003; Courtenay, 2009; COMAB, 2009; Lee & Owens, 2003; MHF, 2010). Good et al. (1989) noted with surprise how little attention had been given in the help seeking literature to male gender roles given they appear to be “intuitively antithetical to the behaviour of help seeking” (Good et al., 1989, p295).
Men who could benefit from professional help may choose not to pursue it because many aspects of psychological help seeking are in direct conflict with dominant masculine gender roles. Psychological therapies often emphasise traits such as emotional expression, introspection, intimacy, and acknowledgement of vulnerability, which may account for fewer men using psychological interventions (Brooks, 1998; Pollack & Levant, 1998; Rochlen, 2005).
In the development and evaluation of the Barriers to Help Seeking Scale with 537 undergraduate males from the US, Mansfield, Addis, and Courtenay (2005) identified five barriers specific to men‟s help seeking, including; the need for control and self reliance; minimising problems and self resignation; concrete barriers and distrust of caregivers; privacy; and emotional control.
Utilisation in the UK
Men show more sporadic and infrequent use of health care services, lack engagement with health material and delay seeking help when faced with health problems (White, Fawkner & Holmes, 2006).
UK statistics indicate that men visit their doctors less frequently than women with the exception of the very young and the very elderly where consultation rates are similar (ISD, 2000; ONS, 2004; NHS Information Centre, 2009; The Scottish Government, 2009).
Women aged between 15 and 44 are twice as likely to visit their GP as men of a similar age (particularly for minor symptoms) and are more likely to be referred for psychological therapy (ISD, 2000; ONS 2000).
A review of progress made by the Improving Access to Psychological Therapies (IAPT) programme showed that men are not accessing psychological therapies at the primary care level as frequently as women. The ratio was just under two women to every one man. The ratios were greater at both age extremes and lowest for people between the ages of 45-54 (Glover, Webb & Evison, 2010; Table 1).
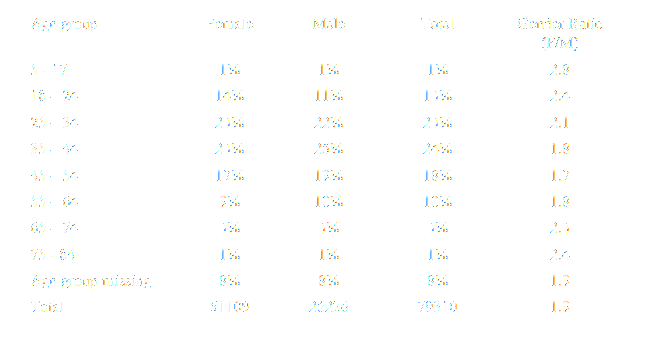
North East Public Observatory Improving Access to Psychological Therapies:
A review of the progress made by sites in the first roll out year
Men become more visible in secondary care mental health services (ONS, 2010) where they are twice as likely to be placed on community treatment orders and make up the vast majority of those detained as mental health inpatients due to prison and court referrals (NHS Information Centre, 2010).
Specific groups of men, such as those from African and Caribbean backgrounds, are more likely to be placed on community treatment orders (NHS Information Centre, 2010) and come into contact with mental health services via the police and criminal justice system (Keating, 2007).
During 2006-2007, 140,000 men used a drug treatment service compared to 55,000 women (NHS Information Centre, 2008).
The figures presented here may indicate that men use less preventative mental health strategies than women and are more likely to come into contact with services when problems are more severe, if at all.
They may also represent a less voluntary use of services and a greater reluctance to seek help from traditional mental health services. Indeed, a scoping study on men‟s health carried out by White (2001) revealed men‟s reluctance to access health care services was a primary issue related to poorer health outcomes for men in the UK.